An Electronic Medical Record (EMR) system is a software platform that allows the electronic entry, storage, and maintenance of digital medical data. From a patient perspective, it is a digital version of a patient’s medical information that would have previously been recorded in a paper chart. Sometimes the term Electronic Health Record (EHR) is used to describe data that includes medical info entered outside of an office or hospital visit. For purposes of this page, I mostly use EMR to describe the clinical and technical components of the software.
EMR systems are used throughout a healthcare organization to document clinical information on many patients over long periods. The systems organize and present data in ways that assist clinicians with interpreting health conditions, with placing orders, and providing ongoing care, scheduling, billing, and follow up.
Data contained in the EMR is also used to create reports for clinical care, disease management, patient communications, and more.
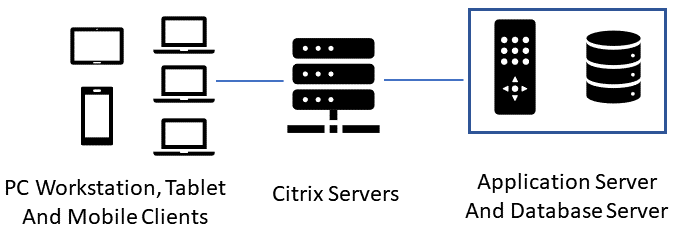
An EMR will typically be accessed by users from a Windows based PC, a tablet, or a Smartphone. Some EMRs are entirely web-based, meaning that the organization using the technology accesses it only from a web browser as opposed to maintaining application servers and database servers. The application and databases are managed and located with the EMR vendor.
Alternatively, many EMRs (especially in large organizations) are not entirely web-based. An example would be a hospital that uses an enterprise wide system such as Epic, Cerner, or MEDITECH. This graphic shows a simplified view of how these EMR systems are configured:
Before the days of EMRs, your medical info was usually entered by hand and by filling out forms in a paper chart binder. Paper charts had a designated order in which the medical information was organized. This is important to cover because the paper chart structure has influenced the workflow and layout of today’s EMRs. Here are the tabs contained in a paper chart:
Face Sheet
A face sheet is a quick view of the patient, containing basic demographic info such as age, gender, address and phone number. It also has an overview of the patient’s medical condition, allergies, and current medications. In an EMR, this overview may be called a Snapshot or Synopsis.
Medical Encounters
This includes events that have occurred in which you interacted with a care provider. Regular office visits, trips to the ER, immunizations, hospital stays, and even telephone calls to your doctor’s office are all encounters, and are recorded in your medical record.
Progress Notes
This is where the physician and other caregivers document their assessment, impressions, and other data observed during visits with patients.
Orders and Prescriptions
Any time a healthcare provider prescribes a medication, orders an X-Ray, or even advises you wear a knee brace- these are all orders and are documented in your medical record.
Test Results
Results from your lab tests, MRIs, or any other diagnostic tests will be in this section.
Other information and documents from other healthcare providers
This is where any miscellaneous documents or materials are kept. For a paper chart, it’s usually near the end.
Medical Documentation – What Gets Entered in the EMR
Now we’ll have a look at what gets entered into the EMR from the time you arrive at the physician’s office, until you check out. Because of the history and logical layout of a paper chart, most EMRs attempt to group electronic data in a similar order to the paper chart. Here is an example of the Kareo system. Notice the tabs on the left indicating the sections of the electronic chart:

Intake – Reason for Visit and Vital Signs
When you arrive in the exam room, the Medical Assistant will open your medical record, usually by clicking on your name from the schedule. They will then confirm what you are being seen for and document it. If you are being seen for abdominal pain, that’s exactly what they will enter in the EMR. It’s important to note that this is not a diagnosis, just a reported observation.Next, vital signs are taken. Federal regulations for Meaningful Use of Electronic Medical Records systems require at least the gathering of height, weight, and blood pressure.
Patient Reported Medications
The MA will then ask you what medications you are on and record them in the EMR. They should ask for name, dosage, strength, and frequency. In the EMR, there will be a medications area that has your current meds list, and a prescriptions area, which has the prescriptions that your doctor may write for you. These are separate areas in the EMR, and the MA typically just documents the reported meds you are taking.
Allergy Documentation
The MA will ask if you are allergic to any substances, foods, or medications. This is one of the most beneficial aspects of an EMR because the systems have built-in allergy and medication conflict checking. Later in the visit, if the physician tries to order a medication that would cause a reaction, they will get a warning.
Medical History and Surgical History
In some care settings, your medical and surgical history may be gathered by the MA, other times it may be gathered by the front desk during check-in. One challenge that still exists with a lot of offices is the tradition of having you fill out a paper form with all of your medical and surgical history, which then seems to go nowhere because you get asked again by someone who keys it into the EMR. This can be solved by having patients enter their history on a tablet or at a kiosk. Medical kiosks are in more and more places these days, but are not quite everywhere yet.
Smoking Status
Another regulatory requirement is to ask all patients about their smoking status and offer smoking cessation materials to current smokers. The MA will record this info into the EMR. We should note that everything entered is date stamped, which is important to meet regulatory requirements that are date sensitive.
The Physician Visit
At this point, the MA will probably log out or secure the PC that is hosting the EMR, or if they are on a tablet, they just leave the room with the tablet. The chart is either considered closed, or secured while you read last year’s magazines and wait for the physician.
When the doctor arrives, they will reopen your chart from the EMR, which will require some form of logging in to validate their identity. They will then take a minute to review the information that the MA entered. What I mentioned in the last section about data-driven regulations applies here as physicians are required to record that they have reviewed various parts of all patients’ medical records. This requirement is usually met by the physician clicking a “mark as reviewed/noted” button that is in several places of the medical record. That action is logged in the database as part of the official record.
Progress Note
The physician will at some point open a progress note section of the record to begin documenting the findings of the visit. Some doctors document while they are visiting with the patient, some start the progress note in between patients, and some document after the visit. It is also sometimes called a SOAP Note.
SOAP stands for Subjective, Objective, Assessment, and Plan. By the names of the sections, you may be able to guess a little about what is contained.
Doctors rarely type the entire contents of the progress note the way we type letters from scratch. Since many of their visits are very similar in structure, they rely on note templates to quickly document their findings. Doctors will usually have note templates for common conditions like flu, ear infections, and respiratory infections. They will also have note templates for certain types of patients, like for an adult physical or a well-child checkup.
Visit Diagnosis
Once the physician has determined the problem, they will enter one or more diagnoses in the EMR. This is not necessarily the same as the chief complaint- many times is isn’t. That’s why they’re the doctors and we’re not. The visit diagnosis is important in the medical record for many reasons, such as:
- Billing: Insurance pays different amounts for different conditions, as we all know,
- Research: If we have accurate diagnoses on many patients, that data can be used to better treat conditions, or even spot trends and potential epidemics.
Diagnoses all have codes that are recognized by clinicians and insurance providers. You may have seen them show up on insurance statements you get in the mail. For example, Type 2 Diabetes has a code of E11.9. An EMR enables physicians to just enter the English description of the code, and have the correct billing equivalent transmitted to insurance providers. Before electronic records, physicians’ offices had to manually keep track of billing codes, and frequently kept huge reference books on hand.
Problem List
Once as diagnosis has been made, the physician will determine if the condition is a long term or chronic condition, like Diabetes. “Flu” would not go on the problem list because it isn’t a long-term condition. Also, usually only the physician has the authority to update diagnoses on the problem list.
Level of Service
Level of service is a code that the physician enters into the chart to correctly bill for various levels of complexity of an office visit. For example, you may have two Diabetes patients; one is managing their condition well with few complications. The other patient is not managing their Diabetes well and has many complications. The more chronic patient visit would be coded to a higher level of service than the other visit.
Medications or Orders
The physician may order medications, lab tests, X-rays, referrals to specialists, or any number of other orders or procedures. Those all have to be entered into the EMR, and each order needs to be associated with the correct diagnosis. Those orders usually have expiration dates and are part of your permanent medical record for historical purposes.
Patient Instructions (After Visit Summary)
When the doctor is finished with the visit, they will usually print an after visit summary (AVS), which is the handout that you get stating what you were seen for and how to address the condition(s). The EMR vendor usually has a component of the software which imports the patient instruction information from a third-party provider of this material. Main suppliers of this integration are RelayHealth and Krames.
Final Medical Documentation Task
The last thing the physician does is to close the encounter in the EMR. This step is very important as many physicians are evaluated on percentage of closed encounters over time. Also, charges for the visit usually cannot be sent electronically to insurance companies until the encounter is closed. At this point, the front desk scheduler may also record the visit as checked out in the EMR.
Post Encounter Billing
While the clinicians are now finished with the encounter, there is usually an electronic transmission that goes to a billing and coding department. The coders will use a combination of software and human analysis to determine any corrections to the encounter before billing is sent to insurance. In some cases, there will be a clinician in the physician department who is also certified in coding. That person may amend the encounter to update the level of service or other billing related areas of the chart.
Scanned Medical Records
For this function, you may have some paper records from outside medical visits that are relevant to your current health that should be included in your record. Most EMRs have the ability to scan these documents into a designated section of the chart. While there is some usefulness to this approach, the contents of the documents is usually not searchable and tends to get forgotten. This is what we call “non-discrete” data, and it’s not the preferred way to capture data.
Benefits of Electronic Health Records
The benefits of electronic health records systems are significant. Prior to electronic records, data was sealed in paper charts that could only be accessed by one person as a time. Each Healthcare provider or location had their own copies of charts that could only be shared between providers by fax, personal courier, or mail. It was a real mess. Some other benefits of electronic health records are:
- The ability to search for data just like you would a website or document;
- The ability to share data and communications with patients and other providers electronically;
- A visual snapshot of the overall condition of a patient, in one view;
- Backups of data that survive natural disasters which could obliterate paper records;
- The ability to store data for detailed analysis of any number of medical conditions or other factors;
- 24/7 access to patient charts via computers or mobile devices.
Challenges of Electronic Health Records
With all the benefits of electronic health records adoption, there are certainly some challenges, as well as complaints from the users:
- The learning curve that comes with the new technology can be a challenge for medical staff who are not used to documenting electronically. While some of the more adept users claim that it makes documentation faster, other users find it takes them longer;
- Added costs are a big deal in the US Healthcare system that is already the most expensive in the world. This has forced most smaller physician practices to sell out to larger organizations who are more able to handle the cost and complexities of EMR implementations;
- Security breaches in Healthcare have increased dramatically in recent years. One 2017 report showed a 305% increase of Healthcare security hacks and ransomware events.

Read More