With the adoption of electronic health records at near universal levels, users of these systems have grown accustomed to having volumes of information on their patients. This has led to clinicians being overloaded with more data than they can reasonably process in the course of providing care. There is a growing need to be able to filter healthcare information in useful ways so that clinicians are presented with the right data on the right patient at the right time. This is where clinical decision support comes in.
Clinical decision support is the answer to this problem and is defined as the ability to provide relevant, contextual information on patients in a way that assists in making informed decisions and taking action on the information provided.
The Centers for Medicare & Medicaid Services (CMS) clarifies that a clinical decision support system should be able to deliver:
- The right information
- To the right people
- Through the right tools
- In the right intervention formats
- At the right points in workflow
The majority of clinical decision support tools are created within the feature sets of the leading EHR systems. The systems will have some form of rules logic that is built to analyze clinical data in real-time, then present advice or alerts to the users of these systems.
A research article published by the Journal of the American Medical Informatics Association showed that clinical decision support tools produced a 53% reduction in sepsis mortality, and an approximate 6% reduction in the 30-day readmission rate.
Clinical Decision Support Examples
Most clinical decision support components are integrated within an organization’s electronic health records system. The technology is configured to present some form of alert or additional information based on the context of what clinicians are doing at the moment, or on demand. Here are some clinical decision support examples used at most healthcare organizations:
Medication interaction and allergy checking
Medication interaction and allergy checking is one of the oldest forms of decision support, and has become a standard feature in all major clinical technologies. EHRs, clinical order entry systems, and medication dispensing systems all have medication interaction, allergy checking, and diagnosis checking built in. When a clinician enters a patient reported medication or prescribes a new medication, the systems check against all known medications, allergies, and diagnoses on the patient to find any potential problems. A strong visual warning is presented to the user that cannot be dismissed without them explicitly acknowledging it. The clinician will usually then do one of three things:
- Cancel the order,
- Select from a list of alternatives,
- Specify a reason for overriding the warning. Sometimes this is valid when the benefit outweighs the risk.
You might be wondering how all of the software vendors stay on the same page regarding medication checking. Drug companies and researchers are finding new interaction and allergy problems all the time, right? Drug interaction data is managed by clinical data clearinghouses that frequently distribute data sets to be imported into the various systems. Two major vendors that provide this data are Wolters Kluwer (Medipsan), and First Data Bank.
Evidence based order sets
Order sets are another well-established implementation of clinical decision support. For example, if a patient is admitted to the hospital with chest pains, specific labs and diagnostic procedures can be grouped into a single order set that a physician signs once for all of the included orders. The EHR can also suggest add-on orders if additional symptoms or conditions are present, and can alert the physician if the same orders were done recently on the patient. All of this helps to ensure the right orders are done at the right time based on established best practices.
Health maintenance reminders
Virtually everyone, healthy or not has things that they need to do at certain stages of life in order to prevent disease and manage their health. Everyone over 50 needs to have a colonoscopy. Patients with diabetes need to have regular eye and foot exams. Women over 45 should have mammograms. All of these kinds of reminders can be presented to physicians and other clinicians within EHR systems, and can be displayed to patients through patient portals.
Actionable reports
All modern EHR systems have robust reporting modules built in that help clinicians and administrators to measure outcomes, manage patient populations, and monitor productivity by users and departments. Along with these reports is the ability to take action on the data that is presented. Here are a couple of examples of how well-designed reports can make a big difference in the delivery of healthcare and patient communications:
- If a medication is recalled, an EHR report can quickly identify all patients on the drug and facilitate communications to all who are affected,
- In the event of a communicable disease outbreak, a report can provide a list of all patients who haven’t had the needed immunizations or who are otherwise at risk.
Lab range alerts
Most lab tests have high and low ranges that require some kind of action when values are recorded outside those thresholds. Clinical decision support tools provide notification to providers through EHR systems and medical devices for patients in various levels of care. It’s important that these kinds of alerts take more than one factor into consideration. A physician would not want a “hair on fire” warning for every patient who has a slightly elevated bilirubin (a liver lab test). However, the ICU staff monitoring a patient in a coma would want to see subtle changes in many different clinical data points. It all depends on the current condition of the patient, the care environment, and other factors.
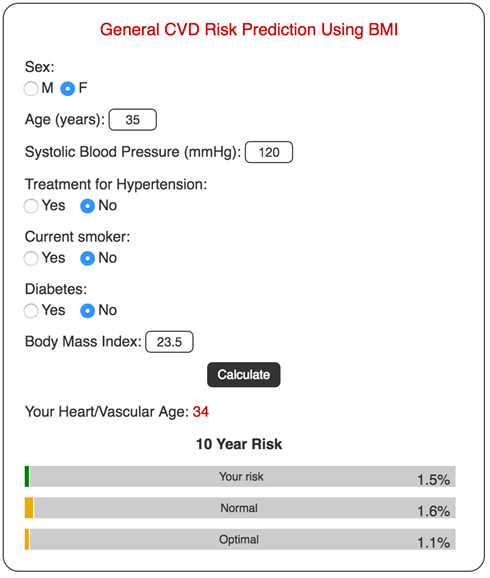
Risk stratification scores
A risk stratification score is a metric that is displayed to clinicians to indicate the likelihood of a patient experiencing a given outcome, such as a re-hospitalization. Risk scores are comprised of components that are assigned different weights and then calculated into an overall score. Some components are the existence of certain diagnoses, lifestyle habits, social factors, numbers and types of medications, or age. Here is an example of a risk stratification score for cardiovascular disease:
Patient specific education resources
When a patient has a medical visit in a hospital or outpatient clinic, the staff usually provides printed materials specific to what they were seen for. This material is configured within the EHR to be filtered from the information that was entered electronically. In the old days, staff had to manually find pre-printed materials to give to patients. This decision support tool makes this job much easier and also provides an electronic accounting that the material was given.
Decision Support In Population Health
Population health strives to improve clinical outcomes for groups of patients. Most of the time, the patient groups are designated by specific traits such as disease, age, gender, geographic region, or socioeconomic status. Some specific examples are:
- Patients with diabetes
- High risk pregnancy patients
- Patients with congestive heart failure
- Patients covered under a specific employer
- Homeless patients
- Patients without a primary care physician
Many different data points are collected on each patient in the respective groups, which helps to identify potential problems with the goal of providing proactive interventions. For example, patients with complex health issues who do not have a primary care provider carry a higher risk of being admitted to the ER with complications that could be prevented. A clinical decision support component can assign a risk score to the patients, giving case managers a clear picture of those who need the most help.

Read More
Developing Clinical Decision Support Tools
When determining what needs to go into any decision support tool, clinicians and operational staff need to ask the right questions to sort out exactly what they are trying to achieve, and how it will affect workflows and the users of EHRs and other technology. Here are some questions to ask when considering a new decision support tool:
- What problem are we trying to solve? An example might be adult patients with a last HbA1c value between 5.7 and 6.4 who have not been seen in over six months need to be reached in order to lower their chances of fully developing type 2 diabetes. This lab test is an indicator of how the body is processing glucose over time, and is critical in managing or preventing type 2 diabetes.
- Where is the data coming from that we are evaluating? We could be getting lab results, diagnoses, demographics or other information from our EHR; and we could also be getting information such as prescription fill history from our electronic prescribing vendor. Various data sources will have different methods for collection and may have different criteria for how they are implemented in a decision support tool.
- Who needs to be alerted when patients meet the criteria, and what tools do we use? We should be looking at the staff who have the opportunity to intervene. We would certainly want high lab values to be seen by the physician during an office visit, but we’re also wanting to proactively reach these patients. So for this example, we would want a report that can be generated to identify our patient group.
- Are there any actions in the EHR or other systems that we want to prevent or “hard-stop”? For our example, we are just using alerts and reports to help identify a segment of patients. However, a surgery encounter would want to verify that the patient has not taken blood thinning medication or fish oil too close to surgery time. This would be a hard stop in a system that needs to be in place to prevent a serious outcome.
- If there are warnings or alerts, should clinicians be able to override them in some cases? This is seen all the time with drug interactions. Just about all medications carry some risk, and those risks may be increased with certain medical conditions. However, sometimes the physician and patient will agree that the benefits outweigh the risks, which means an override should be able to be overridden. The decision support tool would then require a reason for the override.
- How will the outcomes of the decision support tool be measured? In the example of our pre-diabetic patients, we would want to track each outreach attempt and determine if patients are improving over time. Our clinical decision support tool would need to provide this auditing.
Clinical Decision Support Vendors
Clinical decision support is built into all of the major EHR systems such as Cerner, Epic, Meditech, and Allscripts. However, there are other vendors who offer EHR agnostic and stand-alone clinical decision support products. Some of these vendors are Elsevier, Truven Health, and Zynx Health.
Next Up:

Read More


