
As with just about any industry of a significant size, Healthcare IT is affected by, and also affects public policy. Lawmakers at every level get involved in legislation and regulation that affects Healthcare IT. We can’t possibly cover every Healthcare IT policy issue on one page, so let’s look at the major laws that have affected the industry over the years, and look at the role of government in the industry going forward.
Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009
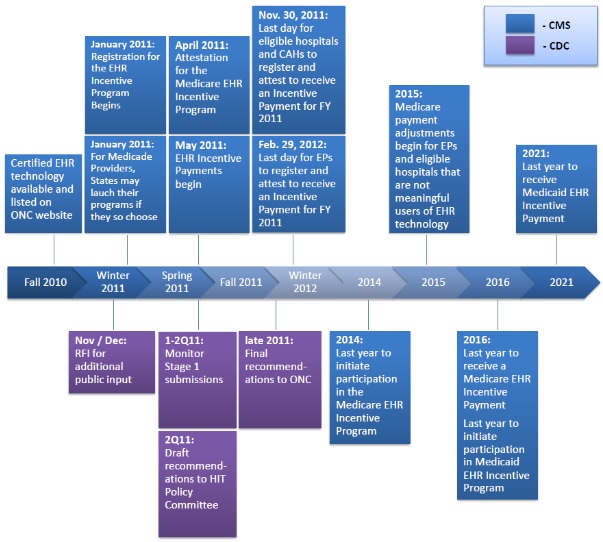
You no doubt have a least a little understanding of the Affordable Healthcare Act of 2010, aka Obamacare. This law does have some Healthcare IT policy components that have affected the industry. However, there is another law that you may not have heard of that more directly affects Healthcare IT. The HITECH Act of 2009 was written to direct all physicians in the U.S. to be on an electronic medical records (EMR) system by 2015. The cost of the program is about $20 Billion. It provided incentives to qualifying physicians of up to about $44,000 per physician running from 2011 through 2016. The payouts depended on physicians documenting that they are using an EMR to a significant enough threshold to make a difference. The term has been labeled Meaningful Use (MU), and it is phased in over three stages. Each stage raises the bar higher than the previous stage in an effort to provided better care to patients. The stages are:
- Stage One – 2011-2012: Data capture and sharing
- Stage Two – 2014: Advance clinical processes
- Stage Three – 2016 and beyond: Improved patient outcomes
If these measures seem complicated and esoteric, to a degree they are. However, many of the specific actions required of physicians are very straightforward, and hard to argue against:
- Offer smoking cessation assistance to smokers, and document that action
- Provide a current list of medications to patients at their office visit
- Provide a web-based patient portal that allows patients to see a summary of their care
Physicians who did not comply with the rules faced financial penalties beginning in 2015 with small reductions in Medicare and Medicaid payments that will increase over time.
Here is a graph from the CDC outlining the timelines:
Some may argue that the Federal Government is overstepping its role by punishing doctors for not getting on electronic health records. I must confess that since I am in this industry, I tend to see the upside of healthcare technology, aware of the many deficiencies that have existed without it. I do take issue with one aspect of HITECH, in that it doesn’t seem to offer any exemption for very small doctor’s offices, i.e. one physician who may only have one other employee. While medium and larger sized practices aren’t having much trouble implementing EMRs, some of these single doctor offices are having a hard time. There are some low-cost systems that claim to be very easy to set up, but that can still be a challenge to a small practice with no IT skills. This has led many independent providers to sell out to large organizations who are better equipped to implement electronic health records.
All in all, as this new world of Healthcare IT unfolds, there are huge opportunities to improve processes and analyze the millions of points of data that will be collected from medical practices.
Affordable Healthcare Act of 2010, aka Obamacare
While much of the healthcare law focuses on getting more people signed up for insurance, there are some aspects that do bring Healthcare IT into the picture. Here are the major Health IT components of Obamacare:
Accountable Care Organizations (ACO)
An accountable care organization is a healthcare system that partners with a group of patients to coordinate care and measure the health of the patient group. Each ACO manages the health of at least 5,000 Medicare beneficiaries for at least three years. The hallmark of this model is that the Providers are not paid exclusively by the services they provide, but by the actual health of the population they serve. For example, if their patients have overall decreased obesity and smoking rates, the Providers are paid bonuses. It’s a pay for performance arrangement. While some may think this is another example of Big Government meddling in peoples’ personal health, remember that the US has one of the poorest performing healthcare systems in the developed world. Canada, Germany, France, and many Asian countries all have longer lives, lower infant mortality, and better outcomes in just about every area of health compared to the US. So the way I see it, this ACO experiment is at least worth a try.
Telemedicine in Rural Areas
Many of American’s health problems are concentrated in rural areas where poverty is higher and communities find it hard to recruit primary care physicians (PCPs). The ACA attempts to address this by expanding the use of tele-medicine. This is where a doctor sees patients via video conferences. The effort got off to a slow start, but in recent years has been gaining traction. Telehealth visits are usually limited to non-complex health issues such as minor infections, colds & flu, and medication refill requests.
Health Information Exchanges (HIE)
In my discussions with friends and family who have no Healthcare IT knowledge, I’ve found that many people think that if they visit a doctor in another state from their primary doctor, all of their medical info is available. In the majority of cases, that is not true, and is one of the reasons that our government has encouraged the Healthcare sector to create Health Information Exchanges (HIEs). An HIE is a technology structure that allows physicians who are not necessarily connected to each other to exchange data about patients. The organizations who participate in an HIE are setup to transmit patient data that is able to be viewed by clinicians located in different areas, who usually use different EMR systems. Many times this data is exchanged on demand to support unplanned care for a patient, such as an ER visit. It is also helpful for patients who have complex chronic conditions that require they visit multiple specialists who are not in the same healthcare networks. I recall one story about a young boy who was being treated at Children’s Hospital Colorado for a complex kidney disease and heart condition. Before electronic health records, his charts filled up one of those red wagons that are used at children’s hospitals. His parents would pull the wagon around the hospital campus to allow the various physicians to then grab the paper records at each visit. Crazy, huh? Once the hospital went digital, his caregivers no longer had to haul around the volumes of paperwork.
21st Century Cures Act of 2016
The 21st Century Cures Act authorized about $6.3 Billion in funds to go toward research, Healthcare quality improvement, the opioid crisis, the FDA drug approval process, and some technology goals. The areas of the law which affect Healthcare IT have to do with:
- Supporting the technical connections between various and competing electronic health records (EHRs) which is commonly referred to as interoperability,
- Improved ability for patients to access their medical records electronically,
- Discouraging information blocking between competing EHR systems,
- Reducing the amount of electronic documentation required by physicians.
Government Healthcare IT Systems
The Veteran’s Administration is the largest provider of Healthcare services in the United States, providing care to over 9 million veterans. The VA developed their own electronic health records system called VistA, which started development in 1977. It was based on technology that is considered antiquated by today’s standards, but it was very impressive in many regards. It included most of the same features and functions of commercial systems, even implementing some components before the private sector had. There is a fantastic article from Politico called A 40 year ‘conspiracy’ at the VA which tells the story of the development of VistA by a somewhat rouge team of physicians and programmers.
The Department of Defense developed its own EHR called AHLTA, the Armed Forces Health Longitudinal Technology Application, which launched in 2004.
However, both VistA and AHLTA are on their way out as these agencies and the Coast Guard have all selected Cerner as their EHR vendor. That system will be branded MHS Genesis, and the first locations were implemented in the Pacific Northwest.
Regardless of which party is at the helm of the three branches of government, we can count on a continued focus on the quality of patient care and outcomes as opposed to Healthcare just being a fee-for-service commodity. That means that EHR technology and data analysis will continue to provide opportunities in the industry for a long time.
Next Up: Learn the common structure of most Healthcare IT systems



